Sleep Apnea
Sleep apnea is a disorder that causes several interruptions in breathing while a person is sleeping. Left untreated, sleep apnea can lead to other health problems such as stroke, heart issues, daytime sleepiness and Type 2 diabetes. This guide explains sleep apnea warning signs, diagnosis and treatment.
What Is Sleep Apnea?
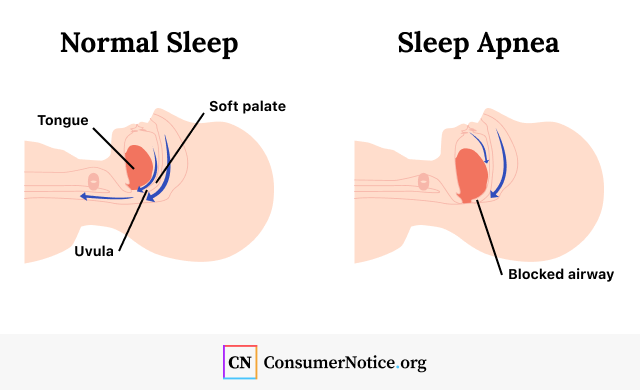
Sleep apnea is a common and potentially serious condition that causes a person to repeatedly stop and start breathing while they are sleeping. It usually happens when the tongue, soft palate or uvula change positions during sleep and block the airway.
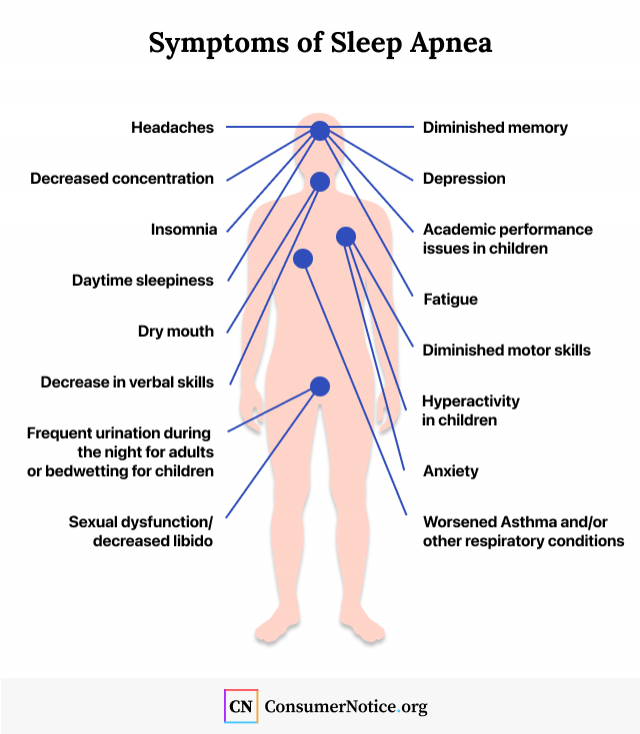
The most common warning signs of sleep apnea are loud snoring or gasping while sleeping and feeling tired even after a full night’s sleep. Morning headaches, dry mouth and trouble staying asleep may also occur.
About 30 million American adults have obstructive sleep apnea, according to the American Academy of Sleep Medicine.
Without treatment, sleep apnea can increase a person’s risk for various health problems such as high blood pressure, fatigue and cardiovascular problems. Fortunately, sleep apnea is highly treatable.
Types of Sleep Apnea
There are three main types of sleep apnea: Obstructive sleep apnea, central sleep apnea and mixed sleep apnea. The most common type is obstructive sleep apnea, or OSA.
- Obstructive (OSA)
- Most people with sleep apnea have OSA. It’s caused when structures in the airway — such as the tongue or uvula — shift and block the airway during sleep. Pauses in breathing usually last for 10 seconds or more and happen five to 30 times each hour. OSA is most common in those who are obese.
- Central
- Central sleep apnea is rarer and happens when the brain fails to signal respiratory muscles to breathe deeply in response to higher levels of carbon dioxide. People with central sleep apnea breathe more slowly and less deeply than normal.
- Mixed
- When people have both OSA and central sleep apnea it’s called mixed sleep apnea. Sometimes, people with OSA develop central sleep apnea while using continuous positive airway pressure (CPAP) treatment.
Signs and Symptoms of Sleep Apnea
The warning signs of sleep apnea can help a person tell if he or she has sleep apnea. Symptoms of sleep apnea are the health problems someone may suffer from the condition.
- Long pauses or reduction in breathing
- Frequent loud snoring
- Choking or gasping for air during sleep
What Causes Sleep Apnea?
Medical conditions, genetics or body structure can cause sleep apnea. The most common cause of sleep apnea is being overweight or obese.
- Genetic Syndromes: Syndromes that affect the shape of the face and skull by causing the tongue to sit farther back in the mouth or cause small facial bones, such as cleft lip or Down syndrome, may lead to sleep apnea.
- Heart or Kidney Failure: Fluid buildup in the neck from these conditions can cause airway blockages.
- Hormone Disorders: Hormone disorders such as hypothyroidism, polycystic ovary syndrome and high levels of growth hormone (acromegaly) are associated with sleep apnea.
- Large Tonsils: Large tonsils may cause narrowing in the upper airway.
- Neuromuscular Conditions: Conditions such as stroke, Chiari malformations, myotonic dystrophy, myasthenia gravis and others may interfere with chest muscles and brain signals to the airway, causing sleep apnea.
- Obesity: Increased fat deposits in the neck can block the airway.
- Premature Birth: Babies born premature have a higher risk of breathing problems, though the risk decreases as they get older, and their brain develops.
Risk Factors
People can control some sleep apnea risk factors such as weight and lifestyle, while other factors, such as age or genetics, can’t be controlled. Make sure you talk to your doctor about your risks and how to prevent sleep apnea.
- Age: Sleep apnea can occur at any age, but it’s more likely to occur in middle-aged and older people.
- Sex: More men than women have sleep apnea, but a woman’s risk increases after menopause.
- Heredity: People with a family history of sleep apnea are more likely to have it. Certain genetic disorders can also increase the risk.
- Lifestyle: Drinking alcohol and using sedatives or tranquilizers can relax the throat muscles and worsen OSA. Smoking increases inflammation in the airway, and smokers are three times more likely to have OSA than nonsmokers.

Sleep Apnea Screening
Medical providers may conduct sleep apnea screenings by using questionnaires that ask patients about potential sleep apnea symptoms such as snoring, high blood pressure and daytime sleepiness. Right now, primary care physicians don’t automatically screen patients for OSA.
When patients bring up potential sleep apnea symptoms to their doctors, they are usually referred to a specialist for diagnosis. However, only about 20% of patients discuss sleep habits with their physicians.
The U.S. Preventive Services Task Force published its sleep apnea screening recommendations in the medical journal JAMA on Nov. 15, 2022. According to the task force, “The current evidence is insufficient to assess the balance of benefits and harms of screening for OSA in the general adult population.”
Without being able to prove that preventative OSA screening has more benefits than harm, the task force doesn’t recommend sleep apnea screening at this time.
How Is Sleep Apnea Diagnosed?
In order to diagnose sleep apnea, your medical provider will check your family history, symptoms and any medical conditions that may contribute to sleep apnea. The provider may check your neck, jaw size, tongue, lungs, heart and neurological systems for potential complications of sleep apnea.
After the physical examination, he or she may prescribe a sleep study, or polysomnography, to diagnose sleep apnea. This is the gold standard for diagnosis. While patients are asleep at a sleep lab, clinicians monitor their blood oxygen, brain waves, heart rate and breathing. After sleep apnea is diagnosed, doctors may perform an endoscopy to identify the location of the airway blockages.
Some doctors may recommend a home test, which can be more convenient than going to a sleep lab, but these tests are less accurate because they only measure breathing. Because they are less accurate, only patients with moderate or severe OSA should use them.
Patients with medical problems such as lung disease, heart failure, hypoventilation, restless leg syndrome or central sleep apnea aren’t candidates for home testing.
What Are My Sleep Apnea Treatment Options?
People diagnosed with sleep apnea might start with lifestyle changes. In some cases, sleep apnea can go away if a patient loses weight, stops smoking and exercises regularly.
If lifestyle changes don’t work, doctors may also recommend implants, oral devices or breathing devices such as a CPAP machine to help people breathe better.
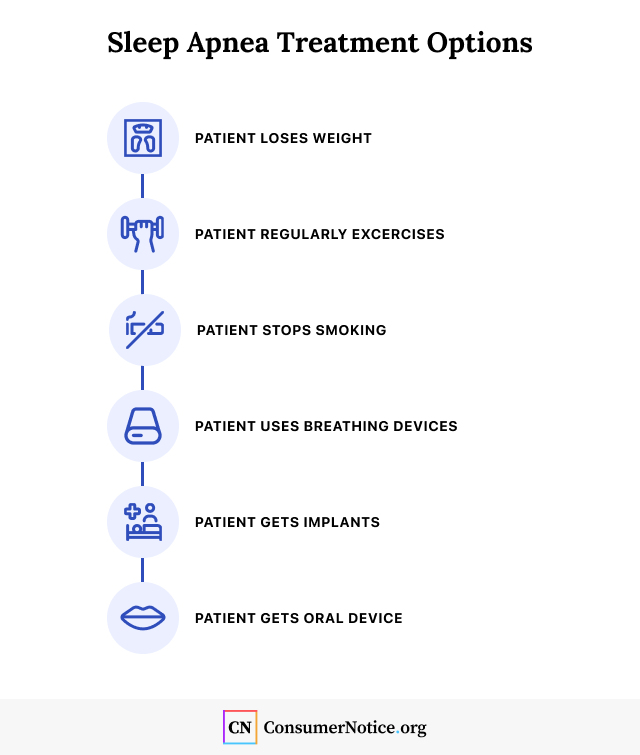
In February 2021, the FDA approved the eXciteOSA device that uses muscle stimulation delivered through a mouthpiece on the tongue to prevent the tongue from collapsing backward. Doctors may also implant a device called Inspire into a patient’s body. When the patient is ready for sleep, they press a button on a remote control and the device helps keep the airway open.
Custom-fit oral devices can reposition the tongue or jaw in order to keep them from blocking airways during sleep.
A CPAP machine is a common treatment for OSA, and many studies have shown it’s effective. CPAP machines generate pressurized air through a facemask that keeps airways open while people are asleep. Some people may not be able to tolerate CPAP side effects. In these cases, doctors may discuss CPAP alternatives with the patient, such as surgery to remove airway blockages.
Philips CPAP Machines Recalled
In June 2021, Philips issued a CPAP recall for several of its machines. Sound abatement foam in the devices may break down and enter the body through the nose or mouth, causing side effects such as cancer and respiratory problems.
Philips is the largest maker of CPAP machines and the recall affected millions of its products.
People who developed cancer and other health problems after using the recalled devices are filing CPAP lawsuits that claim Philips sold a defective device.
What If I Don’t Treat My Sleep Apnea?
Sleep apnea can be a serious condition if left untreated. Some of these complications can be life-threatening. Pauses in breathing cause a decrease in oxygen levels and an increase in blood pressure, which makes the heart work harder. Over time, it can strain the cardiovascular system.
- Asthma
- Atherosclerosis (hardening of the arteries)
- Atrial fibrillation
- Cancers
- Chronic kidney disease
- Cognitive and behavioral disorders
- Gestational diabetes
- Gestational high blood pressure
- Glaucoma
- Glucose intolerance
- Heart attacks
- Heart failure
- High blood pressure
- Keratoconus
- Low birth weight
- Pancreatic damage
- Stroke
- Type 2 diabetes
If you have any signs of sleep apnea, especially loud snoring or gasping while sleeping, make sure to talk to your medical provider.

Sleep Apnea and COVID-19
New studies have also linked obstructive sleep apnea to an increased risk of developing severe COVID-19, but CPAP devices may help reduce the risk.
One such study published in January 2021 in BMJ Open Respiratory Research found that while patients with OSA and those without OSA had a similar risk of contracting the disease, patients with OSA and COVID-19 were more likely to be hospitalized.
In another study, researchers looked at more than 80,000 health records and found people with untreated OSA had a higher risk of infection than people without OSA. But CPAP therapy may reduce an OSA patient’s risk of infection, according to data presented at the American Thoracic Society’s 2021 International Conference.
13 Cited Research Articles
Consumernotice.org adheres to the highest ethical standards for content production and references only credible sources of information, including government reports, interviews with experts, highly regarded nonprofit organizations, peer-reviewed journals, court records and academic organizations. You can learn more about our dedication to relevance, accuracy and transparency by reading our editorial policy.
- Kaltwasser, J. (2021, May 25). Sleep Apnea Appears to Increase Risk of COVID-19 Infection. Retrieved from https://www.ajmc.com/view/sleep-apnea-appears-to-increase-risk-of-covid-19-infection
- U.S. Food and Drug Administration. (2021, February 5). FDA Authorizes Marketing of Novel Device to Reduce Snoring and Mild Obstructive Sleep Apnea in Patients 18 Years and Older. Retrieved from https://www.fda.gov/news-events/press-announcements/fda-authorizes-marketing-novel-device-reduce-snoring-and-mild-obstructive-sleep-apnea-patients-18
- Strausz, S. et al. (2021). Sleep apnoea is a risk factor for severe COVID-19. Retrieved from https://bmjopenrespres.bmj.com/content/8/1/e000845
- U.S. National Library of Medicine. (2021, August 2). Sleep Apnea. Retrieved from https://medlineplus.gov/sleepapnea.html
- Cleveland Clinic. (2020, March 3). Sleep Apnea. Retrieved from https://my.clevelandclinic.org/health/diseases/8718-sleep-apnea
- US Preventive Services Task Force. (2022, November 15). Screening for Obstructive Sleep Apnea in Adults: US Preventive Services Task Force Recommendation Statement. Retrieved from https://jamanetwork.com/journals/jama/fullarticle/2798399
- Strohl, K.P. (2020). Sleep Apnea. Retrieved from https://www.merckmanuals.com/home/lung-and-airway-disorders/sleep-apnea/sleep-apnea
- American Academy of Sleep Medicine. (2019, August 6). Six facts about sleep apnea. Retrieved from https://sleepeducation.org/six-facts-about-sleep-apnea/
- Joy, K. (2016, March 18). When Is a Home Sleep Apnea Test Appropriate? Retrieved from https://labblog.uofmhealth.org/rounds/when-a-home-sleep-apnea-test-appropriate
- Mayo Clinic. (n.d.). Sleep apnea. Retrieved from https://www.mayoclinic.org/diseases-conditions/sleep-apnea/symptoms-causes/syc-20377631
- Stanford Health Care. (n.d.). Obstructive Sleep Apnea Diagnosis: How Do I Know I Have OSA? Retrieved from https://stanfordhealthcare.org/medical-conditions/sleep/obstructive-sleep-apnea/diagnosis.html
- Inspire. (n.d.). How it Works. Retrieved from https://getstarted.inspiresleep.com/
- National Heart, Lung, and Blood Institute. (n.d.). Sleep Apnea. Retrieved from https://www.nhlbi.nih.gov/health-topics/sleep-apnea
Calling this number connects you with a Consumer Notice, LLC representative. We will direct you to one of our trusted legal partners for a free case review.
Consumer Notice, LLC's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.
844-420-1914



