Acid Reflux and GERD Medicine
Acid reflux and GERD medicine lower stomach acid to manage symptoms. There are three main types of medications available over-the-counter and as prescriptions. These are: Antacids, H2 blockers and proton pump inhibitors. This guide will help you understand what causes acid reflux and GERD and the pros and cons of each medication.
Acid Reflux vs. GERD
Acid reflux, also known as gastroesophageal reflux (GER) or heartburn, happens when the contents of the stomach travel back up into the esophagus. GERD, or gastroesophageal reflux disease, is a more serious, long-lasting form of acid reflux. Left untreated it can lead to scarring in the esophagus or esophageal cancer.
Acid reflux is common. More than 60 million Americans experience heartburn at least once a month, according to the American College of Gastroenterology. At least 15 million Americans experience heartburn each day.
GERD is also common. About one in five American adults has GERD, according to the International Foundation for Gastrointestinal Disorders.
“An incredibly [large] proportion of the U.S. population has experienced these symptoms at some point and many will use [acid reflux and GERD] medications,” Dr. Caleb Alexander, a professor at Johns Hopkins Bloomberg School of Public Health and practicing internist, told Consumer Notice.

Fortunately, acid reflux and GERD are highly treatable. Depending on the severity of symptoms, medical providers will decide the best drugs and treatment plan for each patient. They may also recommend lifestyle changes such as diet and exercise to control symptoms.
In order to make the best medication choice, it’s important to understand what causes acid reflux and GERD.
Acid Reflux
Acid reflux happens when stomach acid backs up into the esophagus from the stomach. It’s common and can happen to anyone from time to time.
The main symptom of acid reflux is heartburn, and people sometimes use the terms interchangeably. Heartburn feels like a burning discomfort behind the breastbone. It can move up to the neck or throat and can cause a sour or bitter taste. The symptoms of heartburn may last for hours and get worse when people eat.
Acid reflux that happens two or more times a week may be a sign of a more serious problem called GERD.
Acid Reflux Diet
For some people, changes in diet can help control symptoms and decrease their dependence on medication.
Certain foods can trigger heartburn and make it worse. It’s best to avoid these foods. Foods high in fat, salt and spices sit in the stomach longer and increase the risk of acid reflux.
- Bacon, sausage and other fatty meats
- Carbonated beverages
- Cheese
- Chili powder
- Chocolate
- Fast food
- Fried food
- Fruits in the citrus family (oranges, lemons, limes)
- Pepper (white, black, cayenne)
- Peppermint
- Pizza
- Processed snacks such as potato chips
- Tomato-based sauces
“Dietary modification is often one of the first approaches used to manage heartburn and reflux. All too often we reach for pharmacologic treatment while neglecting to consider often very effective behavioral approaches that can be used to manage symptoms such as heartburn and reflux,” Alexander said.
Eating to Avoid Acid Reflux
Making small changes to your diet can help control acid reflux symptoms. Doctors recommend eating smaller, more frequent meals and avoiding big meals and snacks close to bedtime.
- Whole grains such as oatmeal or brown rice
- Sweet potatoes, carrots and other root vegetables
- Green vegetables
- Low acid fruits such as bananas, cauliflower, nuts and melons
- Watery foods such as herbal tea, watermelon, celery, cucumber and lettuce
Eating foods that are high in fiber, alkaline foods and watery foods can help stave off heartburn, according to Gupta. Incorporating more of these foods may help control stomach acid.
GERD
GERD is a more serious version of acid reflux. If your heartburn happens two times a week or more, you may have GERD.
Certain medicines such as calcium channel blockers for high blood pressure, some asthma medicines, nonsteroidal anti-inflammatory drugs (NSAIDs), benzodiazepines and tricyclic antidepressants can cause GERD or make symptoms worse.
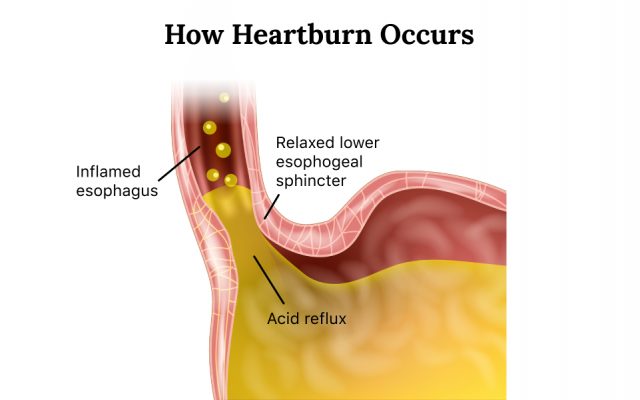
In people with GERD, the lower esophageal sphincter — the muscle that separates the stomach from the esophagus — relaxes too frequently and lets stomach acid, digestive enzymes and other materials flow back up into the esophagus.
People who have had a hiatal hernia, are pregnant, who smoke or are overweight have a greater risk of having GERD.
GERD Symptoms
People with GERD experience the same symptoms of people with acid reflux. But they also suffer from more serious and uncomfortable symptoms. For example, having GERD at night can disrupt sleep.
- Chest pain
- Chronic cough
- Difficulty swallowing
- Disrupted sleep
- Feeling like there is a lump in your throat
- Heartburn after eating that is worse at night
- Laryngitis
- New or worsening asthma
- Regurgitation of food or sour liquid
Without treatment, GERD can increase the risk of esophageal cancer and esophagitis that may cause ulcers and bleeding in the esophagus.
GERD Diet
People who have GERD should follow guidelines similar to the acid reflux diet to reduce heartburn attacks. There is no proven GERD diet, but eating certain foods may ease your symptoms. Discovering a diet that works for you may involve a lot of trial and error. Ask your doctor for a nutritionist that may be able to help.
- Sit up with good posture while eating and avoid lying down for at least two hours after a meal.
- Avoid alcohol. It weakens the lower esophageal sphincter and irritates the stomach.
- Stand up and walk after a meal. It helps gastric juices flow in the right direction.
- Try to eat your last meal of the day at least three hours before bed.
- Keep a diary of foods that trigger your GERD symptoms so you can avoid them or reduce the amount you eat.
- Chewing gum (not spearmint or peppermint) increases saliva production and reduces acid in the esophagus.
Avoid high-fat foods, chocolate, caffeine, carbonated beverages and alcohol. Focus on foods high in fiber and low in fat. Examples include lean meats, complex carbohydrates, vegetables and healthy fats from fish, nuts and olive oil.
Common Medications for Acid Reflux and GERD
If diet and lifestyle choices don’t improve your acid reflux and GERD symptoms, a doctor may recommend medication. Acid reflux and GERD medicine is available over-the-counter (OTC) and by prescription.
These medications come in three main types: antacids, H2 blockers and proton pump inhibitors or PPIs.

“Many people who have mild or intermittent symptoms of reflux may be able to take over-the-counter treatments alone. Frankly, patients can often self-manage that with little to no clinical input, but many other patients may have more severe GERD symptoms or more complex GI disease, such as gastritis or erosive esophagitis or gastrointestinal ulcers — which we don’t see often, but they still can occur — are times when a prescription treatment makes more sense,” said Alexander.
| Medication Type | How Long They Work | OTC or Prescription | Common Side Effects |
|---|---|---|---|
| Antacids – Tums, Rolaids, Mylanta, Maalox | They work in about five minutes but only last 30 to 60 minutes. | OTC for mild heartburn. They’re not intended to treat GERD or severe acid reflux | Mild side effects such as nausea, diarrhea, constipation |
| H2 Blockers – Tagamet, Zantac (withdrawn from the market), Pepcid | They work in about 30 minutes and control acid for about 12 hours. | OTC and prescription for acid reflux and GERD | Diarrhea, constipation, headache, muscle aches and abdominal pain |
| Proton Pump Inhibitors – Prilosec, Protonix, Prevacid and Nexium | They can take one to four days to start working but last for up to 24 hours. | OTC and prescription for the most severe cases of acid reflux and GERD | Headache, abdominal pain, nausea, diarrhea and flatulence |
If heartburn is mild and only happens occasionally, people can use weaker OTC medicines such as antacids. For more serious acid reflux or GERD, medical providers may prescribe stronger medicines such as H2 blockers or PPIs. Weaker medicines like antacids don’t treat GERD.
“H2 blockers are generally used for more mild disease. For people that require more complete acid suppression, proton pump inhibitors are superior,” Alexander said.
Which Medicine Is the Safest?
In general, medications for acid reflux and GERD are safe for most people. But all medications have side effects and no medicine is 100% safe for everyone. Some medicines have fewer and milder side effects.
According to Alexander, patients should always ask their provider if they have questions about safety. Providers will help patients decide which medications are the safest and most effective for them.
“In some cases, there are many people taking these medicines that don’t even need them. For some people, the medicine could be discontinued outright, but these judgements should be made in consultation with a health care provider. And then other instances, people may elect either to stay on their medicine aware of the risks or switch to an alternative medicine,” he said.
What’s the Risk of Cancer from NDMA Contamination in Zantac?
In April 2020, the U.S. Food and Drug Administration told all drug makers to withdraw all Zantac and generic ranitidine products from the market because it found N-Nitrosodimethylamine (NDMA) in some batches of the drug.
NDMA is a chemical known to cause cancer in animals and may cause cancer in humans. Animal studies have demonstrated the carcinogenic effects of NDMA and the International Agency for Research on Cancer (IRAC) has classified it as a probable human carcinogen (group 2A).
So far, the FDA hasn’t reported any cases of cancer linked to Zantac, but some people filed Zantac lawsuits against drug manufacturers after they took the drug and developed cancer. Many of these people did not have a family history of the disease or genetic markers for increased risk, according to lawyers.
- Bladder cancer and bladder removal
- Breast cancer
- Colon cancer
- Esophageal cancer
- Kidney cancer and kidney removal
- Liver cancer
- Melanoma
- Ovarian cancer
- Prostate cancer
- Stomach cancer
“I think it’s understandable that many people may have concerns about these safety issues,” Alexander said. “The good news is that the absolute risk to any individual exposed to these products is exceedingly small. And there are lots of other treatment options when it comes to managing heartburn, reflux and other GI diseases.”
PPIs and Serious Side Effects
PPIs are powerful acid reducers, and overall most people don’t have problems when taking them. But they can cause serious side effects in some people, especially if they take them long-term. Over the counter PPIs are recommended only for 14 day cycles but prescriptions can be up to 8 weeks.
“Both H2 blockers and proton pump inhibitors are generally well-tolerated classes of medicine. While the potential for uncommon, adverse effects is always there, generally these medicines are well-tolerated and their use is not limited by any adverse effects,” Alexander said.

Some side effects that rarely occur with PPI long-term use include the risk of fractures, Clostridium difficile bacterial infections and gastric malignancies.
PPIs can also increase the chance of serious kidney problems such as chronic kidney disease and acute interstitial nephritis, or swelling inside the kidney, according to the National Kidney Foundation. People with kidney problems shouldn’t take PPIs. This side effect has led to PPI lawsuits.
When Should I Call my Doctor about Drug Side Effects?
Many drugs come with a medication insert that has a long list of side effects. For some patients, this can be just as confusing as it is helpful, according to Alexander.
“I think it’s best to err on the side of caution. So I think it’s best for patients to reach out when they have a specific concern. Clinicians can provide assistance to patients in helping them to understand what they should look for when they are taking a new medicine,” he said.
He stresses that ensuring patients get the best health care is a partnership between a provider and the patient. Providers are always available to help.
“Any medicine can be overused, and the last thing we need is more people taking medicines that they don’t need. I think this is the art and science of medicine — figuring out why someone needs a medicine and getting them the right medicine at the right time. Patients shouldn’t feel as though they have to make these decisions alone.”
8 Cited Research Articles
Consumernotice.org adheres to the highest ethical standards for content production and references only credible sources of information, including government reports, interviews with experts, highly regarded nonprofit organizations, peer-reviewed journals, court records and academic organizations. You can learn more about our dedication to relevance, accuracy and transparency by reading our editorial policy.
- American College of Gastroenterology. (n.d.). Acid Reflux. Retrieved from https://gi.org/topics/acid-reflux/
- International Foundation for Gastrointestinal Disorders. (2019). Introduction to GERD. Retrieved from https://www.aboutgerd.org/introduction-to-gerd.html
- International Foundation for Gastrointestinal Disorders. (2019). Diet Changes for GERD. Retrieved from https://www.aboutgerd.org/diet-lifestyle-changes/diet-changes-for-gerd.html
- Johns Hopkins Medicine. (n.d.). GERD Diet: Foods That Help with Acid Reflux (Heartburn). Retrieved from https://www.hopkinsmedicine.org/health/wellness-and-prevention/gerd-diet-foods-that-help-with-acid-reflux-heartburn
- National Institute of Diabetes and Digestive and Kidney Disorders. (2020, July). Symptoms & Causes of GER & GERD. Retrieved from https://www.niddk.nih.gov/health-information/digestive-diseases/acid-reflux-ger-gerd-adults/symptoms-causes
- National Institute of Diabetes and Digestive and Kidney Disorders. (2020, July). Definition & Facts for GER & GERD. Retrieved from https://www.niddk.nih.gov/health-information/digestive-diseases/acid-reflux-ger-gerd-adults/definition-facts#common
- National Kidney Foundation. (2016, March 8). Acid Reflux and Proton Pump Inhibitors. Retrieved from https://www.kidney.org/atoz/content/acid-reflux-and-proton-pump-inhibitors
- U.S. Food and Drug Administration. (2020, April 1). FDA Requests Removal of All Ranitidine Products (Zantac) from the Market. Retrieved from https://www.fda.gov/news-events/press-announcements/fda-requests-removal-all-ranitidine-products-zantac-market
Calling this number connects you with a Consumer Notice, LLC representative. We will direct you to one of our trusted legal partners for a free case review.
Consumer Notice, LLC's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.
844-420-1914

