Hernia Mesh
Hernia mesh is a net-like implant that prevents organs, tissue or fat from bulging through weak muscle walls. While 90% of groin hernia repairs use mesh, complications can include pain, hernia recurrence and infection. Hernia mesh materials and surgical techniques used affect complication rates.
Hernia Mesh and Hernia Surgery
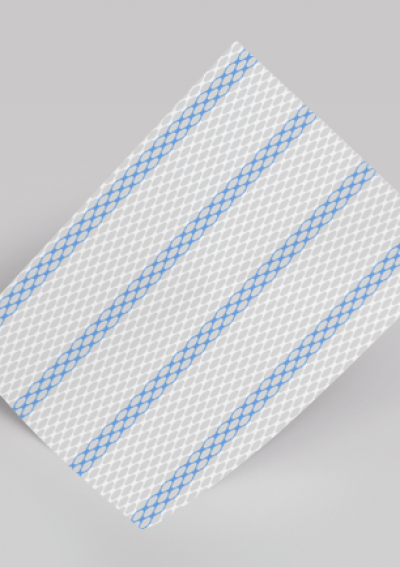
Hernia mesh is a net-like implant, often made from polypropylene plastic, treats hernias. It prevents the tissue, organs or fat from bulging through weak muscle walls. Doctors commonly use mesh to treat patients with hernias because of the low hernia recurrence rate.
- According to the Food and Drug Administration, doctors in the U.S. treat 1 million inguinal hernia every year and use hernia mesh in about 90% of these cases.
- More than 20 million hernia surgeries occur worldwide each year, with 1 million relying on meshes.
- Statistics show the complication rate for mesh is between 12% and 30%.
While typically a safe procedure, there are possible complications, including infection, chronic pain, hernia mesh failure and hernia recurrence. These can lead to additional surgeries. Patients should discuss possible complications and surgery alternatives with their doctors.
Pros and Cons of Using Hernia Mesh
Hernia mesh can successfully repair hernias, but there is the possibility of complications. Infection, for example, is a risk. One study found that when infected hernia mesh was tested, staphylococcus aureus was present in 64% of those cultures, meaning staphylococcus aureus was the primary driver of the tested mesh infections.
- Lower rate of hernia recurrence
- Mesh can repair larger weak areas
- Decreased operative and recovery time
- Mesh can migrate, shrink or cause other complications
- Mesh may get infected, requiring removal
- Mesh failure requires one or more revision surgery
Sometimes, the risks of hernia mesh may outweigh the benefits. The likelihood and severity of complications depend on the material of the mesh, the surgeon and surgical technique and the response of the patient’s body.
Research estimates that less than half of patients choosing mesh repair require repair surgeries, with non-mesh or suture-based repairs experiencing higher recurrence rates. The ideal hernia mesh resists infection and an inflammatory response, while staying flexible and quickly incorporating into the body’s tissue.
How Long Does Hernia Repair Last?
Non-absorbable hernia repair mesh should be a permanent fix, but absorbable mesh typically dissolves in six to 18 months. Hernia recurrence is possible even with non-absorbable mesh.
Research suggests that mesh materials may affect recurrence rates after hernia repair. Polypropylene mesh is extremely durable, but because of its heavy weight, it can lead to inflammation in the area. This has a shrinking effect on the mesh, creating higher recurrence rates.
Hernia Mesh Complications
The FDA is aware of complications arising from recalled meshes and current market products. While many people experience improved quality of life following hernia treatment, others report mild to serious complications.
- Adhesion: Unwanted attachment of the mesh to loops of the bowel or other tissue
- Bowel obstruction: Perforation of the intestines that creates a blockage
- Hernia recurrence: Reappearance of a hernia at the original site
- Mesh migration: Movement because of poor adhesions or pressure
- Mesh shrinkage: Shrinking mesh that pulls on tissue and causes pain
- Persistent pain: Discomfort or pain near the leg, groin, abdomen, stomach or testicles
- Seroma: Painful lump or mass of clear fluid
- Sexual problems: Erectile dysfunction and pain
- Wound infection: Infections occurring around the site
You may experience symptoms such as fever, flu-like symptoms, nausea, vomiting or constipation. Other signs of hernia mesh failure include chronic pain and severe swelling or tenderness at the surgery site.
Hernia mesh failure can happen a few weeks or a few years after your surgery. Talk to your doctor as soon as you notice something wrong or out of the ordinary after your hernia surgery.
Types of Hernia Mesh
Hernia mesh materials fall into different categories: Synthetic, biological, coated, composite and hybrid meshes. Mesh is available in different weaves, sizes and strengths and is available as patches, plugs and sheets.
This indicates that type of mesh may be associated with outcomes, and mesh choice could therefore depend on hernia type.
Different mesh materials lead to different rates of complications. In an April 2023 meta-analysis, researchers formed a conclusion that biologic meshes increase the complications of surgery site infections and hernia recurrences. As an alternative, uncoated, macroporous synthetic mesh is suitable for open ventral hernia repair.
Absorbable or Biologic Hernia Mesh
Biologic hernia mesh uses animal or human donor tissue, often decellularized intestines or skin of cows and pigs. The material breaks down over time and absorbs into the body.
A surgeon may choose this mesh for a strangulated hernia or if there is an infection in the location. Recurrence is a potential complication.
Non-Absorbable or Synthetic
With a synthetic mesh, a surgeon could use a woven or nonwoven sheet. These materials remain in the body indefinitely and include polyester, polypropylene or expanded polytetrafluoroethylene. These types of mesh are chemically inactive and should minimize reaction complications.
While polypropylene is one of the more common mesh materials, it can wear away or break down over time. If this occurs, the mesh could protrude or cause injury to surrounding tissue.
Hybrid, Coated or Composite
These materials have non-absorbable or absorbable coatings such as cellulose, beta glucan, omega-3 fatty acids or collagen. The coatings minimize the body’s inflammatory response.
A leading benefit of choosing a coated or composite mesh is the ability of surgeons to use it in intraperitoneal space with little adhesion formation risk. Studies show varying degrees of inflammation risk from composite mesh, depending on the materials used.
Glue vs Suture
Glue fixation had shorter operating time and lower haematoma formation than suture fixation. Chronic pain and seroma formation were comparable.
Evidence to support less chronic pain with glue is not very strong. It mostly comes from the shorter operating time and less trauma during the procedure.
Hernia Mesh Recalls and Market Withdrawals
Several manufacturers voluntarily withdrew or recalled their hernia mesh from the market. Some actions were initiated because of packaging errors, higher than normal failure rates or the risk of serious complications such as adhesions, pain and hernia recurrence.
- December 2020: Ethicon, Inc. issued a recall on the Proceed surgical mesh device because a hair was found inside the packaging of a unit.
- March 2019: ACell, Inc recalled Gentrix Surgical Matrix Thick because a sample from the lot failed to meet company tensile strength specifications.
- November 2018: Covidien LLC recalled Parietex Composite Parastomal Mesh after receiving reports of parastomal mesh failure.
- October 2018: Covidien/Medtronic recalled its Parietex Composite Parastomal Mesh for mesh failure occurrences.
- August 2016: Novus Scientific issued a recall to add to the product’s instructions and present additional information relating to clinical study results.
A company will voluntarily withdraw a product when the violation is minor and not subject to legal action from the FDA. A drug or device recall occurs when there is evidence or a belief that the product is harmful or defective.
Hernia Mesh Brands and Manufacturers
There are currently more than a dozen major hernia mesh manufacturers dominating the U.S. market. Product options come in various sizes across brands.
| Manufacturer | Products Lines and Brands |
|---|---|
| Atrium | C-QUR, Vitamesh, Proloop, Prolite, Prolite Ultra |
| Autosuture | Surgipro |
| B. Braun | Sefil, Premilene |
| C.R. Bard/Bard Davol | 3DMax, AlloMaxBard Soft Mesh, Bard Mesh Sheets, CollaMend, Composix, Dulex, Kugel, MK Patch, OnFlex, PerFix Plug, Phasix Mesh, Phasix, Sepramesh IP Composite, Ventralex, Ventralight, Ventrio, Visilex, XenMatrix Surgical Graft |
| Cook Medical | Surgisis |
| Covidien/Medtronic | Parietene, Parietex, Permacol, ProGrip, Symbotex, Versatex, Prolene Light, Optilene, Permacol |
| Ethicon/Johnson & Johnson | FlexHD Structural, Mersilene, Physiomesh, Proceed, Proline, Ultrapure, Ultrapure Advanced, Vicryl, XCM Biologic, Vypro, Vypro II |
| FEG Textiltechnik | Dynamesh |
| Genzyme | Sepramesh IP Composite |
| GfE | Ti-Mesh |
| Gore Medical | Bio-A, Dual mesh, Micromesh, Gore-Tex Soft Tissue Patch, Sinecure |
| LifeCell | Strattice |
| Meadox | Trelex |
| Syneture | Dexon |
Manufacturers that issued a recall for one or more of their hernia mesh products include Atrium Medical, Bard Davol, Ethicon/Johnson & Johnson and Covidien/Medtronic. If you have questions about which hernia mesh was used in your surgery, your surgeon’s office will be able to confirm that information for you.
Hernia Mesh Lawsuits Filed Over Complications
Thousands of hernia mesh lawsuits accuse manufacturers of producing devices that caused serious complications. Four major mesh makers are at the center of separate multidistrict litigations, large court actions that combine similar lawsuits in a single federal court. In MDLs, plaintiffs receive a portion of the settlement award, often based on the severity of their case.
Active Hernia Mesh MDLs
Active Hernia Mesh MDLs
| Atrium Medical | |
|---|---|
| Brands Named | C-QUR |
| MDL Location | New Hampshire District |
| Pending Lawsuits | 758 |
| Expected Trial Dates | In settlement |
| Ethicon | |
|---|---|
| Brands Named | Physiomesh Flexible Composite Hernia Mesh |
| MDL Location | Georgia, Northern District |
| Pending Lawsuits | 26 |
| Expected Trial Dates | In settlement |
| Bard Davol | |
|---|---|
| Brands Named | All polypropylene mesh brands |
| MDL Location | Ohio, Southern District |
| Pending Lawsuits | 24,115 |
| Next Expected Trial Date | April 2024 |
| COVIDIEN | |
|---|---|
| Brands Named | All hernia mesh brands |
| MDL Location | Massachusetts |
| Pending Lawsuits | 1,511 |
| Expected Trial Dates | To be determined, motions to appear issued 2023 |
Hernia mesh manufacturers often settle out of court with plaintiffs to avoid going to trial. In February 2023, the Attorney General for the state of Kentucky announced that Ethicon settled litigation for close to $10 million.
45 Cited Research Articles
Consumernotice.org adheres to the highest ethical standards for content production and references only credible sources of information, including government reports, interviews with experts, highly regarded nonprofit organizations, peer-reviewed journals, court records and academic organizations. You can learn more about our dedication to relevance, accuracy and transparency by reading our editorial policy.
- U.S. Judicial Panel on Multidistrict Litigation. (2024, January 2). MDL Statistics Report - Distribution of Pending MDL Dockets by District. Retrieved from https://www.jpml.uscourts.gov/sites/jpml/files/Pending_MDL_Dockets_By_Actions_Pending-January-2-2024.pdf
- FDA. (2023, July 13). Surgical Mesh Used for Hernia Repair: Information for Patients. Retrieved from https://www.fda.gov/medical-devices/hernia-surgical-mesh-implants/hernia-surgical-mesh-implants-information-patients
- Poli de Figueiredo, S.M. et al. (2023, April). Biologic versus synthetic mesh in open ventral hernia repair: A systematic review and meta-Analysis of randomized controlled trials. Retrieved from https://www.surgjournal.com/article/S0039-6060(22)01030-3/fulltext
- Birolini, C. et al. (2023, February 9). Microbiology of chronic mesh infection. Retrieved from https://link.springer.com/article/10.1007/s10029-023-02747-6
- Baker, J.J., Oberg, S. & Rosenberg, J. (2023, February). Reoperation for Recurrence is Affected by Type of Mesh in Laparoscopic Ventral Hernia Repair. Retrieved from https://journals.lww.com/annalsofsurgery/Abstract/2023/02000/Reoperation_for_Recurrence_is_Affected_by_Type_of.24.aspx
- FDA. (2022, December 21). Class 2 Device Recall Proceed Surgical Mesh. Retrieved from https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfres/res.cfm?id=184219
- Wang, Z. et al. (2022, November 29). Plasma-Induced Diallyldimethylammonium Chloride Antibacterial Hernia Mesh. Retrieved from https://pubs.acs.org/doi/10.1021/acsabm.2c00695
- Jangjoo, A., Kalantari, M.E. & Zandbaf, T. (2022, September 2). Mesh migration following abdominal hernia repair: A case report, and literature review. Retrieved from http://caspjim.com/article-1-2970-en.html
- Aziz, S.S. et al. (2022, July 13). Comparison of Early Outcomes in Patients Undergoing Suture Fixation Versus Tack Fixation of Mesh in Laparoscopic Transabdominal Preperitoneal (TAPP) Repair of Inguinal Hernia. Retrieved from https://www.cureus.com/articles/103296-comparison-of-early-outcomes-in-patients-undergoing-suture-fixation-versus-tack-fixation-of-mesh-in-laparoscopic-transabdominal-preperitoneal-tapp-repair-of-inguinal-hernia
- Tanushree, S. et al. (2022, July). A review of recent developments of polypropylene surgical mesh for hernia repair. Retrieved from https://www.sciencedirect.com/science/article/pii/S2352952022000093
- Ayuso, S.A. et al. (2022, July). Coated Polypropylene Mesh Is Associated With Increased Infection in Abdominal Wall Reconstruction. Retrieved from https://www.sciencedirect.com/science/article/abs/pii/S0022480422000464
- Layer, T. et al. (2022, May 10). Incisional hernia repair with a slowly absorbable P4HB mesh: what happens after the mesh disappears? A retrospective longitudinal clinical study. Retrieved from https://link.springer.com/article/10.1007/s10029-022-02616-8
- Whittaker, R. et al. (2022, March 1). Emergent and Urgent Ventral Hernia Repair: Comparing Recurrence Rates Amongst Procedures Utilizing Mesh Versus No Mesh. Retrieved from https://link.springer.com/article/10.1007/s00464-022-09101-4
- Smith, S.M. et al. (2022, April 21). Mesh versus non-mesh repair of groin hernias: a rapid review. Retrieved from https://onlinelibrary.wiley.com/doi/10.1111/ans.17721
- Rosen, M.J. et al. (2022, April 1). Biologic vs Synthetic Mesh for Single-stage Repair of Contaminated Ventral Hernias: A Randomized Clinical Trial. Retrieved from https://jamanetwork.com/journals/jamasurgery/fullarticle/2788222
- Phoa, S. (2022, February 3). Comparison of glue versus suture mesh fixation for primary open inguinal hernia mesh repair by Lichtenstein Technique: a systematic review and meta-analysis. Retrieved from https://link.springer.com/article/10.1007/s10029-022-02571-4
- Wilson, R.B. & Farooque, Y. (2022, January 21). Risks and Prevention of Surgical Site Infection After Hernia Mesh Repair and the Predictive Utility of ACS-NSQIP. Retrieved from https://link.springer.com/article/10.1007/s11605-022-05248-6
- Attaar, M. et al. (2021, July). Mesh in Elective Hernia Repair: 10-Year Experience with over 6,000 Patients. Retrieved from https://journals.lww.com/journalacs/abstract/2021/07000/mesh_in_elective_hernia_repair__10_year_experience.10.aspx
- Harris, H.W. et al. (2021, April 1). Preventing Recurrence in Clean and Contaminated Hernias Using Biologic Versus Synthetic Mesh in Ventral Hernia Repair: The PRICE Randomized Clinical Trial. Retrieved from https://journals.lww.com/annalsofsurgery/abstract/2021/04000/preventing_recurrence_in_clean_and_contaminated.7.aspx
- Madsen, L.J. et al. (2020, June). Mesh Versus Suture in Elective Repair of Umbilical Hernia: Systematic Review and Meta-Analysis. Retrieved from https://academic.oup.com/bjsopen/article/4/3/369/6061450
- Wang See, C., Kim, T. & Zhu, D. (2020). Hernia Mesh and Hernia Repair: A Review, Retrieved from https://www.sciencedirect.com/science/article/pii/S2666138120300025
- Ssentongo, A.E. et al (2019, November 14). Pain and Dysfunction with Sexual Activity after Inguinal Hernia Repair: Systematic Review and Meta-Analysis. Retrieved from https://journals.lww.com/journalacs/abstract/2020/02000/pain_and_dysfunction_with_sexual_activity_after.8.aspx
- Gomez-Gil, V. et al. (2019, February 27). Evaluation of Synthetic Reticular Hybrid Meshes Designed for Intraperitoneal Abdominal Wall Repair: Preclinical and In Vitro Behavior. Retrieved from https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0213005
- FDA. (2019, January 15). Medical Device Recalls Database. Retrieved from https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfRes/textsearch.cfm
- Branley, A. (2018, December 1). Hernia Mesh Concerns Grow Among Men as More Patients Report Surgery Complications. ABC News (Australia). Retrieved from https://www.abc.net.au/news/2018-12-02/hernia-mesh-concerns-grow-among-men-surgery-complications/10570182
- Elghali, M.A. et al. (2018, November 1). Unusual Complication of Seroma After Ventral Hernia Mesh Repair: Digestive Perforation by Tacks. A Case Report. Retrieved from https://www.sciencedirect.com/science/article/pii/S2210261218304681?via%3Dihub
- FDA. (2018, October 5). Class 2 Device Recall Parietex Composite Parastomal Mesh. Retrieved from https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfRES/res.cfm?id=168668
- Wise, J. (2018, September 27). Hernia Mesh Complications May Have Affected Up to 170 000 Patients, Investigation Finds. Retrieved from https://www.bmj.com/content/362/bmj.k4104
- Kulacoglu, H. (2018, July 1). Comments on the New Groin Hernia Guidelines: What Has Changed? What Has Remained Unanswered? Turkish Journal of Surgery. Retrieved from https://www.turkjsurg.com/abstract/1568/eng
- Zargar, N. &and Carr, A. (2018, June 19). The Regulatory Ancestral Network of Surgical Meshes. PLOS One. Retrieved from https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0197883
- FDA. (202318, JulyFebruary 134). Hernia Surgical Mesh Implants. Retrieved from https://www.fda.gov/medical-devices/implants-and-prosthetics/hernia-surgical-mesh-implants
- Kockherling, F. et al. (2018, January 31). What Is the Evidence for the Use of Biologic or Biosynthetic Meshes in Abdominal Wall Reconstruction? Retrieved from https://link.springer.com/article/10.1007/s10029-018-1735-y
- HerniaSurge Group. (2018, January 12). International Guidelines for Groin Hernia Management. Hernia. Retrieved from: https://link.springer.com/article/10.1007%2Fs10029-017-1668-x
- Wise, J. (2018). Hernia Mesh Complications May Have Affected Up to 170 000 Patients, Investigation Finds. Retrieved from https://www.bmj.com/content/362/bmj.k4104.full
- BMJ News. (2017, September 27). Hernia Mesh Complications May Have Affected up to 170,000 Patients, Investigation finds. The BMJ. Retrieved from https://www.bmj.com/content/362/bmj.k4104.full
- Elango, S. et al. (2017, September 7). Mesh Materials and Hernia Repair. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5571666/
- Baylon, K. et al. (2017, August 22). Past, Present and Future of Surgical Meshes: A Review. Retrieved from https://www.mdpi.com/2077-0375/7/3/47
- Elango, S. et al. (2017, August 25). Mesh materials and hernia repair. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5571666/
- Kontogiannis, S., Goulimi, E., &and Giannitsas, K. (2016, October 18). Reasons for and Against Use of Non-absorbable, Synthetic Mesh During Pelvic Organ Prolapse Repair, According to the Prolapsed Compartment. Retrieved from https://link.springer.com/article/10.1007/s12325-016-0425-3
- Kokotovic, D., Bisgaard, T., and Helgstrand, F. (2016, October 18). Long-Term Recurrence and Complications Associated with Elective Incisional Hernia Repair. JAMA. Retrieved from https://jamanetwork.com/journals/jama/fullarticle/2565771
- Science Daily. (2016, October 18). Study finds mixed results for use of mesh for hernia repair. Retrieved from https://www.sciencedaily.com/releases/2016/10/161018094928.htm
- Nikkolo, C. &and Lepner, U. (2015, November 15). Chronic Pain After Open Inguinal Hernia Repair. Postgraduate Medicine. Retrieved from https://www.tandfonline.com/doi/abs/10.1080/00325481.2016.1121090
- Narkhede, R. et al. (2015, June 27). Postoperative Mesh Infection—Still a Concern in Laparoscopic Era. Retrieved from https://link.springer.com/article/10.1007/s12262-015-1304-x
- Lockhart, K., et al. (2015). Mesh Versus Non-Mesh for Inguinal and Femoral Hernia Repair. Cochrane Database of Systematic Reviews. Retrieved from https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD011517/epdf/full
- Sternschuss, G., Ostergard, D.R., and Patel, H. (2012, May 12). Post-Implantation Alterations of Polypropylene in the Human. Journal of Urology. Retrieved from https://www.auajournals.org/doi/10.1016/j.juro.2012.02.2559
Calling this number connects you with a Consumer Notice, LLC representative. We will direct you to one of our trusted legal partners for a free case review.
Consumer Notice, LLC's trusted legal partners support the organization's mission to keep people safe from dangerous drugs and medical devices. For more information, visit our partners page.
855-877-5976

